Sickle Cell Disease and the Gap in the Blood Supply -How the First and Most Common Genetic Disease in the United States is still a Major

Health Concern
According to the CDC and NIH, Sickle cell affects almost all ethnicities; primarily affecting people with ancestors from Africa, India, Central and South America, the Middle East, the Caribbean and Mediterranean countries such as Italy, Greece and
Turkey. Sickle Cell disease is actually the most common genetic blood disease in the United States with approximately 100,000 people of various racial and ethnic backgrounds affected, most of whom are of African or Latino descent. It was first discovered in 1910 in the United States, but the mutation appeared in Africa and India thousands of years ago and eventually appeared in other regions of the planet. The common denominator with these locations is that they are or were at one point a malaria zone. Believe it or not, this mutation actually served as protection for some people against deadly diseases such as malaria.
What many people are unaware of is the frequency at which a patient with sickle cell disease relies on blood transfusion. Whether pediatric or adult, single patient can receive up to 100 pints of blood each year. Sickle cell disease causes red blood cells to be hard and crescent-shaped instead of soft and round. As a result, blood has difficulty
flowing smoothly and carrying oxygen to the rest of the body, which may lead to severe pain, tissue and organ damage, anemia and even strokes. Getting
transfused blood allows the organs, including the brain to function properly. It is also important to note that 1 in every 13 Black or African Americans are born with the
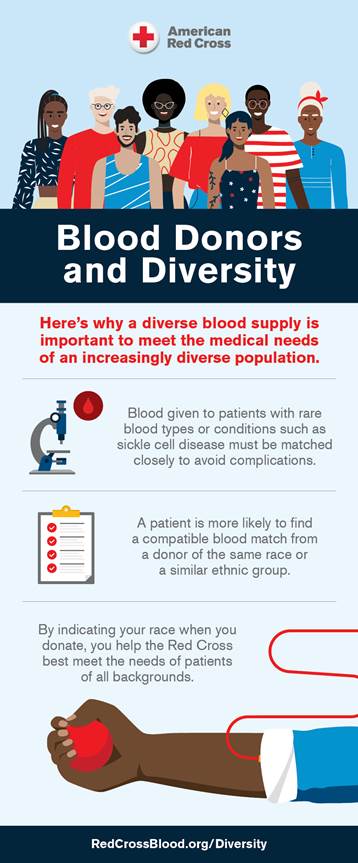
trait for sickle cell. Donate Blood and Identify Your Race
The American Red Cross Biomedical Services currently provides in-depth testing,
typing and matching of blood products for people with sickle cell disease. To better serve people with sickle cell disease—a disease that disproportionately affects Black and African Americans—we’re proud to announce a new campaign that will focus on collecting more blood
products from donors of Black, Latino and African American backgrounds. Black and Latino
blood donors are also important to the overall blood supply because there is a higher frequency
of Type O blood within this demographic of our population than any other ethnicity. This blood
type is most requested by our trauma units and hospital partners for life threatening bleeding
emergencies caused by a traumatic injury such as a life threatening injury to a major organ or
puncture to a major artery, gun shots, car accidents, life threatening surgical procedures, and
childbirth complications.
The goal of the Close the Sickle Cell Gap strategy and campaign is to cultivate a larger pool of diverse blood donors. Black and African American donors are key to the lifesaving treatment patients with sickle cell disease rely on. This is relevant because these donors are more likely than other demographics to have blood specific properties best suited to alleviate the painful symptoms of sickle cell disease in most patients. Well-matched blood can decrease the risk of complications related to transfusion therapy, especially in patients who receive lifelong transfusions. It is critical to increase the number of available blood donors from all racial and ethnic groups. Blood Transfusions provide a lifesaving treatment for patients during a sickle cell crisis by
increasing the number of normal red blood cells in the body which help to deliver oxygen throughout the body and unblock blood vessels. Having a larger pool of Black and African American donors is critical to the quality of care and treatment these
patients receive. Blood from individuals of similar ethnic background can prevent alloimmunization and will increase the chances of having more closely matched blood in order to increase the number of patients with sickle cell disease we can serve. Having a diverse blood supply is a reflection of our diverse population and we are committed to making sure all patient needs have the chance of being met.
To learn more, or inquire about hosting a lifesaving blood drive in your
community, please contact Meosha Hudson, Regional Diversity Account
Manager at 410-375-5190 or Meosha.hudson@redcross.org.

Data and Statistics provided by: The National American Red Cross, Centers for Disease Control and the
National Institute of Health